An Ode to Sodium Hypochlorite
Some would say there’s no money in endodontic irrigation solutions. And, to be quite honest, we’d agree. We’re not telling you to throw out the fancy schmancy $110/bottle solution focus-grouped by many degrees in marketing, but…
Though much of the focus on endodontic treatment has been on instrumentation – every year we see new and improved products released with promises of easier, more efficient treatment and implied greater success – the endodontic literature even dating back to our founding fathers stresses the importance of irrigation. We don’t need India Ink or a microscope to tell us that canals are not perfectly round. That neato Chinese finger trap instrument heavily promoted at dental meetings a few years ago, that promised to instrument every canal crevasse has gone the way of Pogs and faded into the deep abyss. And anyway, was that really going to help us get into the miniscule isthmuses that we pretend don’t exist but may harbor all of the bugs and debris that can cause endodontic failure?
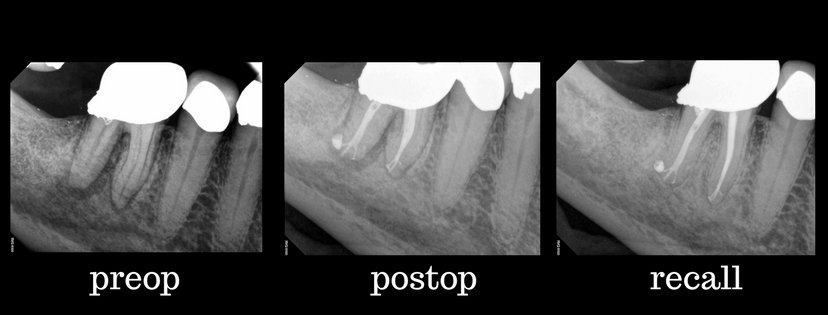
Beautiful healing where instruments simply could not reach, courtesy of sodium hypochlorite, EDTA and sonic activation!
You know what will? Irrigation! Irrigants that have strong antimicrobial action! Irrigants that dissolve organic tissue! And, can you image if we activate these with sonic or ultrasonic waves?
Sodium hypochlorite can do all these things – and more! And, it is just about the most readily available, and least expensive dental material out there. Amazon sells a 30 oz container of Chlorox regular bleach for $7.49. (Perhaps they’ll raise the price once all you dentists increase demand!) Using 10 cc per procedure, this bottle will cover just over 88 cases at a cost of $0.08 per case. You guys, this is using TOP SHELF, BRAND NAME stuff. Your patients will be so impressed.
Now, the nitty gritty. Sodium hypochlorite, better than any other available irrigant solution today, dissolves both necrotic and vital tissue, as well as other organic components of the smear layer (Rosenfeld, James et al. 1978, Baumgartner and Mader 1987). It has strong antimicrobial capabilities, including superior abilities over other irrigants to address E. faecalis (Morgental, Singh et al. 2013), a notoriously difficult to kill endodontic bug, and it can penetrate into Fort Knox-like biofilm structures (Del Carpio-Perochena, Bramante et al. 2011). Full strength hypochlorite better penetrates biofilms (Stojicic, Shen et al. 2013), and it is safe to use with side-vented irrigation needles (Harrison, Baumgartner et al. 1981). Sodium hypochlorite should be used in generous quantities, and the solution should be changed frequently during its use, as dentin can neutralize the active ingredient, the chlorine ion, in about 60 seconds (Arias-Moliz, Morago et al. 2016).
Sodium hypochlorite does lack the ability to address inorganic tissue and therefore the mineralized components of the smear layer. For this, we recommend the adjunct of ethylenediaminetetraacetic acid, more readily called EDTA as a final rinsing agent (Calt and Serper 2002). We advise against alternating between sodium hypochlorite and EDTA given that mixing results in inactivation of the chlorine ion (Baumgartner and Mader 1987) and can even result in excessive dentin demineralization when hypochlorite is used as a final rinse following EDTA (Qian, Shen et al. 2011). Therefore, we recommend using sodium hypochlorite for initial access and instrumentation followed by EDTA as a final rinse just before obturation. The additional use of some degree of passive ultrasonic irrigation or sonic activation has been shown to improve both debridement and disinfection of canals (Jensen, Walker et al. 1999), and we use this routinely as an adjunct to increase the efficacy of our dear old sodium hypochlorite and EDTA.
References
Arias-Moliz, M. T., A. Morago, R. Ordinola-Zapata, C. M. Ferrer-Luque, M. Ruiz-Linares and P. Baca (2016). “Effects of Dentin Debris on the Antimicrobial Properties of Sodium Hypochlorite and Etidronic Acid.” J Endod 42(5): 771-775.
Baumgartner, J. C. and C. L. Mader (1987). “A scanning electron microscopic evaluation of four root canal irrigation regimens.” J Endod 13(4): 147-157.
Calt, S. and A. Serper (2002). “Time-dependent effects of EDTA on dentin structures.” J Endod 28(1): 17-19.
Del Carpio-Perochena, A. E., C. M. Bramante, M. A. Duarte, B. C. Cavenago, M. H. Villas-Boas, M. S. Graeff, N. Bernardineli, F. B. de Andrade and R. Ordinola-Zapata (2011). “Biofilm dissolution and cleaning ability of different irrigant solutions on intraorally infected dentin.” J Endod 37(8): 1134-1138.
Harrison, J. W., C. J. Baumgartner and D. R. Zielke (1981). “Analysis of interappointment pain associated with the combined use of endodontic irrigants and medicaments.” J Endod 7(6): 272-276.
Jensen, S. A., T. L. Walker, J. W. Hutter and B. K. Nicoll (1999). “Comparison of the cleaning efficacy of passive sonic activation and passive ultrasonic activation after hand instrumentation in molar root canals.” J Endod 25(11): 735-738.
Morgental, R. D., A. Singh, H. Sappal, P. M. Kopper, F. V. Vier-Pelisser and O. A. Peters (2013). “Dentin inhibits the antibacterial effect of new and conventional endodontic irrigants.” J Endod 39(3): 406-410.
Qian, W., Y. Shen and M. Haapasalo (2011). “Quantitative analysis of the effect of irrigant solution sequences on dentin erosion.” J Endod 37(10): 1437-1441.
Rosenfeld, E. F., G. A. James and B. S. Burch (1978). “Vital pulp tissue response to sodium hypochlorite.” J Endod 4(5): 140-146.
Stojicic, S., Y. Shen and M. Haapasalo (2013). “Effect of the source of biofilm bacteria, level of biofilm maturation, and type of disinfecting agent on the susceptibility of biofilm bacteria to antibacterial agents.” J Endod 39(4): 473-477.


